What we know:
1. Autopsy results show alveolar-capillary micro-thromboses are nine times as prevalent in the patients who died from COVID-19 compare to deaths from H1N1.
2. Thrombosis is a prevelant feature in multiorgan injuries. It is prominent in the pulmonary micro-vasculatures, alveolar capilaries approaching 90% of the times.
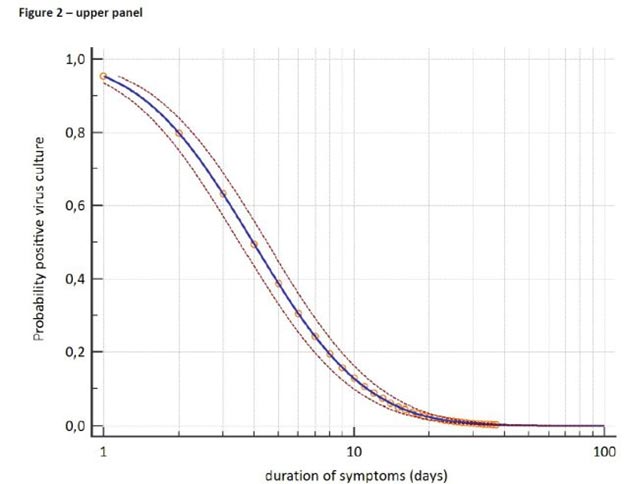
Timelines of recovering replicable SARS COV -2 from the upper respiratory tract.
(Graph derived from published numerical data provided by CDC)
Discussion:
While inflammatory dysregulations and microvascular thrombosis may account for mortality risks, the micro-vascular thrombosis could be contributing to both mortality and long term morbidity. These primary pathophysiologies are progressive on a daily basis. Most patients developing dyspnea by D#7 while entering severe to critical phase at D#10.
From what we know thus far, we can divide COVID-19 into two phases:
- Viral Phase until D#7 of symptoms
- Inflammatory and Thrombotic Phase, beyond D#7.
This framework give us a model for a targeted therapeutic approach:
INPATIENT PROTOCOL (LOVEDEX+)
Acute care medicine has decades of experience using high dose steroids e.g. Solumedrol in some cases 1g/day * 3 days followed by steroid taper over weeks. In several diseases such as COPD, asthma and COPD exacerbations, Glomerulonephritis, IBD, etc. We typically use steroids higher dosages than the 6mg daily of dexamethasone ( Equivalent of 34mg a day of Methylprednisolone) what we currently give for Cytokine storms.
Other considerations:
Inpatient Daily Labs
CBC, CMP, D- Dimer, CRP, Ferritin, Fibrinogen, LDH and Vitamin D Hydroxy
However D Dimer & CRP seems more useful predictors of recovery.
Should consider daily CRP monitoring as it rises with any COVID complications ( Bacterial superimposed infections, Penumothoraxes, pneumomediastimum, etc.)
Imaging
Should consider CT chest w/o IV contrast. Low threshold to repeat if clinical pictures worsened since bacterial pneumonia, Pneumomediatnium and penumothoraxes are frequent.
Daily declines of D-Dimer and CRP normalize are reassuring, while CRP uptrend may indicate bacterial complications.
Imaging by CT scan in this fashion documents improvement and in a baseline for possible pulmonary fibrosis/scaring seen in severe COVID -19 pneumonia.
Oxygenation improvements lag resolution of inflammatory markers by 36-48 hours. As an adjuvant principle, keep patients fluid balance negative as possible.
OUTPATIENT and ER DISCHARGE PROTOCOLS (XarDex+)
The COVID-19 crisis has reminded us that it is quite easy to overwhelm a nation’s hospital system. In countries with limited hospital and ICU resources at baseline, any strategy to treat patients early on and as an outpatient, would be beneficial. It is a kin of treating pneumonia or any bacterial infections to that matter, early on not deffering it until sepsis developes.
I have experience with such patients. I have found it prudent and safe to give anti-inflammatory plus anticoagulant agents before the pulmonary phase of the illness (D#7 and beyond), to prevent advancement of the disease. Dexamethasone when given at Days # 5, 6 and latest 7 of symptoms seems to be beneficial in blocking the take off and progressions of the inflammatory Tsunami. Steroids however before D # 5 is reported to be harmful as it hampered the immune systems abilities to clear the Virus. The key aspect of this approach is to pinpoint the 1st day of symptom onset in high risk groups.
Reference links:
https://www.nejm.org/doi/full/10.1056/NEJMoa2015432.1,2
https://www.cdc.gov/coronavirus/2019-ncov/community/strategy-discontinue-isolation.html
Timeline of Symptoms of Severe Coronavirus Disease 2019 (Covid-19)
https://doctorimuro.com/wp-content/uploads/2020/07/Megakaryocytesandplatelet-in-COVID-19.pdf

